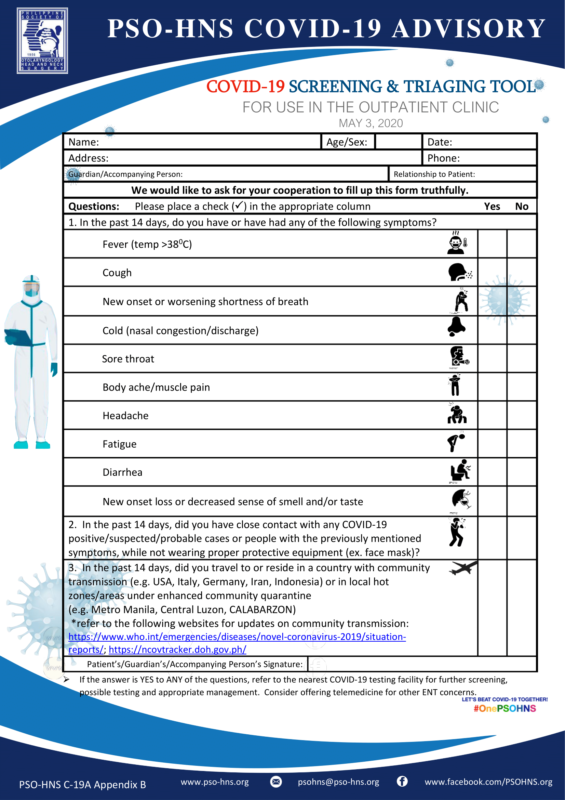
“Erratum: Changes were made to the OPD workflow full text and Appendix B – Screening and Triage Tool to include sore throat which was missed out in the previous release.”
Otolaryngologists are among the health care workers with the highest risk of being infected with SARS-CoV-2 since it is inherent in our practice to examine the areas known to have high viral loads (i.e. nose, nasopharynx, oropharynx). The use of instrumentation in these areas may also aerosolize the virus thus increasing the risk of transmission. Although triaging patients with COVID-19 symptoms to the appropriate health care facility may minimize risk at the clinic, there is still the possibility of asymptomatic virus carriage.
It is therefore prudent to treat all patients as possibly infected, and to take measures to protect the healthcare workers, and other patients. The use of personal protective equipment (PPE) was already discussed in an earlier advisory, so this will focus more on the administrative measures that otolaryngologists can put in place in the OPD to minimize exposure risk.
Recommendations on ORL-HNS Patient Screening and Clinic Workflow
- Prepare to safely screen and manage otolaryngology-head and neck disease patients by doing an inventory of clinic resources and working within its threshold capacity. It is also useful to update with current scientific SARS-Cov-2 infection prevention and control measures and guidance/advisories from the Department of Health (DOH), local government advisories, and your hospital/institution. Be mindful of unfounded opinions and news items.
- To lessen virus transmission, prevent ER patient surges, and save on medical resources (e.g. PPE), telemedicine or virtual patient care is highly encouraged among otolaryngologist- head and neck surgeons. Guidance for telemedicine has been set by the Department of Health and the National Privacy Commission (Joint DOH-NPC Memorandum Circular No. 2020-00016 entitled “Guidelines on the Use of Telemedicine in COVID-19 Response”).
- When patient care cannot be achieved by telemedicine and/or when evaluation procedures are necessary for decisions with regard to timely and urgent case management, in-person or face-to-face clinic encounters may be done by the otolaryngology-head and neck surgeon based on his/her clinical judgment, following triaging and safety precautions to reduce the risk of disease transmission.
- The otolaryngologist-head and neck surgeon and clinical assistants should use appropriate protective personal equipment (PPE), perform proper donning and doffing procedures depending on the infection risk stratification based on DOH, local government advisories and/or institutional recommendations.
PRE-CLINIC VISIT
- All patients should be seen at the clinic on an APPOINTMENT BASIS.
- To be able to obtain an appointment, an initial screening via telemedicine (e.g., phone call, and/or video call) should be done.
- If the patient responds YES to ANY of the following questions, refer him/her to the nearest COVID-19 testing facility for further screening, possible testing and appropriate management.
a. In the past 14 days, do you have or have had any of the following symptoms?
- Fever (temp >380C)
- Cough
- New onset or worsening shortness of breath
- Cold (nasal congestion/discharge)
- Sore throat
- Body ache/muscle pain
- Headache
- Fatigue
- Diarrhea
b. In the past 14 days, did you have close contact with any COVID-19 positive/suspected/probable cases or people with the previously mentioned symptoms, while not wearing proper protective equipment (ex. face mask)?
c. In the past 14 days, did you travel to or reside in a country with community transmission (e.g. USA, Italy, Germany, Iran, Indonesia) or in local hot zones/areas under enhanced community quarantine (e.g. Metro Manila, Central Luzon, CALABARZON)
*refer to the following websites for updates on community transmission:
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports
4. If the patient answers NO to ALL the items above, you may proceed to set the appointment for an in-office visit. Alternatively, if the otolaryngologist-head and neck surgeon is able to meet the patient’s needs via telemedicine, then there is no urgent need for an in-office visit.
CLINIC VISIT
- ALL PATIENTS, whether new or follow-up patients, who arrive at the clinic need to undergo screening by the receiving staff (e.g., guard, receptionist, clinic assistant, nurse). Patients who have previously been screened via telemedicine should still undergo screening. Aside from the symptom and travel history check, vital signs should be obtained, paying particular attention to temperature, respiratory rate, and oxygen saturation (if available).
- A NO MASK, NO ENTRY policy should be implemented. This is aligned with the IATF guidelines on wearing masks when out in public.
- Alcohol hand rub or hand-washing should be done by all patients and companions after going through the footbath (if available), prior to reaching the reception desk.
- As much as possible, companions should not be allowed inside the clinic. Only persons with disability, children needing supervision, or persons needing obvious assistance (e.g., very pregnant women, etc.) will be allowed a companion inside the clinic. The companion must also pass the screening measures instituted by the clinic.
- The waiting area should have proper physical distancing (i.e. at least 6 feet or 2 meters) between seats. There should be no toys, reading materials, or other shared objects in the waiting area, to decrease the risk of contamination. Prepare a system wherein, as much as possible, only one patient at a time is at the waiting area (i.e. limit patient appointments, only one doctor at a time using a shared clinic space). Consider having patients wait in their car, if possible, and inform them via SMS once it is their turn.
- Periodic disinfection should be done for all high-touch surfaces (e.g., desks, door knobs/handles, seat, reception table, ballpens, BP cuff and stethoscope, etc.) using either 0.5% (5000ppm) chlorine or 70% alcohol or other disinfectants recommended by the institutional infection control. Refer to the following website for an updated list of disinfectants useful against SARS-COV-2: https://www.epa.gov/pesticide-registration/list-n-disinfectants- use-against-sars-cov-2
- The nose, nasopharynx and oropharynx are known to carry high loads of SARS-COV-2 virus, thus it is recommended to reduce unnecessary examination in these areas, including procedures that may cause aerosolization. If aerosol-generating procedures (AGP) are necessary, these should be performed in a dedicated “dirty” room equipped with a negative pressure system.
- There should be a designated area for donning and doffing PPE, particularly the lab gown or bunny suit. Prepare designated closed containers for PPE to be discarded and those to be reused. There should also be accessible closed trash bins, preferably with foot pedal, for use by the patient and clinic staff.
References:
- Adre F. Department of Otorhinolaryngology-Head & Neck Surgery Protocol: OPD Operation in COVID Environment.
- American Academy of Family Physicians. AAFP Checklist to Prepare Physician Offices for Covid-19. [Internet] Available from: https://www.aafp.org/dam/AAFP/documents/patient_care/public_health/COVID-19% 20Office%20Prep%20Checklist.pdf
- Center for Disease Control and Prevention. Outpatient and Ambulatory Care Settings: Responding to Community Transmission of COVID-19 in the United States. [Internet] [Last reviewed: April 7, 2020]. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/ambulatory-care-settings.html
- Dimaguila GAC. OPD Clinic Manual in the Time of Covid. ORLHNS Manilamed Medical Center Manila.
- Tay JK, Lim WS, Loh WS, Loh KS. Commentary: Sustaining Otolaryngology services for the long haul during the COVID-19 pandemic: Experience from a tertiary health system. [Internet] [cited 2020 April 13] Available from: https://www.entnet.org/sites/default/files/uploads/tay_sustaining_otolaryngology_ser vices_for_the_long_haul_during_the_covid-19_pandemic.pdf.
- University of Cape Town Division of Otolaryngology. CORONAVIRUS: Update for the ENT Surgeon. [Internet] [cited 2020 April 13] Available from: https://www.globalchildrenssurgery.org/wp-content/uploads/2020/04/67-UCT_COVID- 19_Otolaryngology_ENTAfrica_Guidelines.pdf.